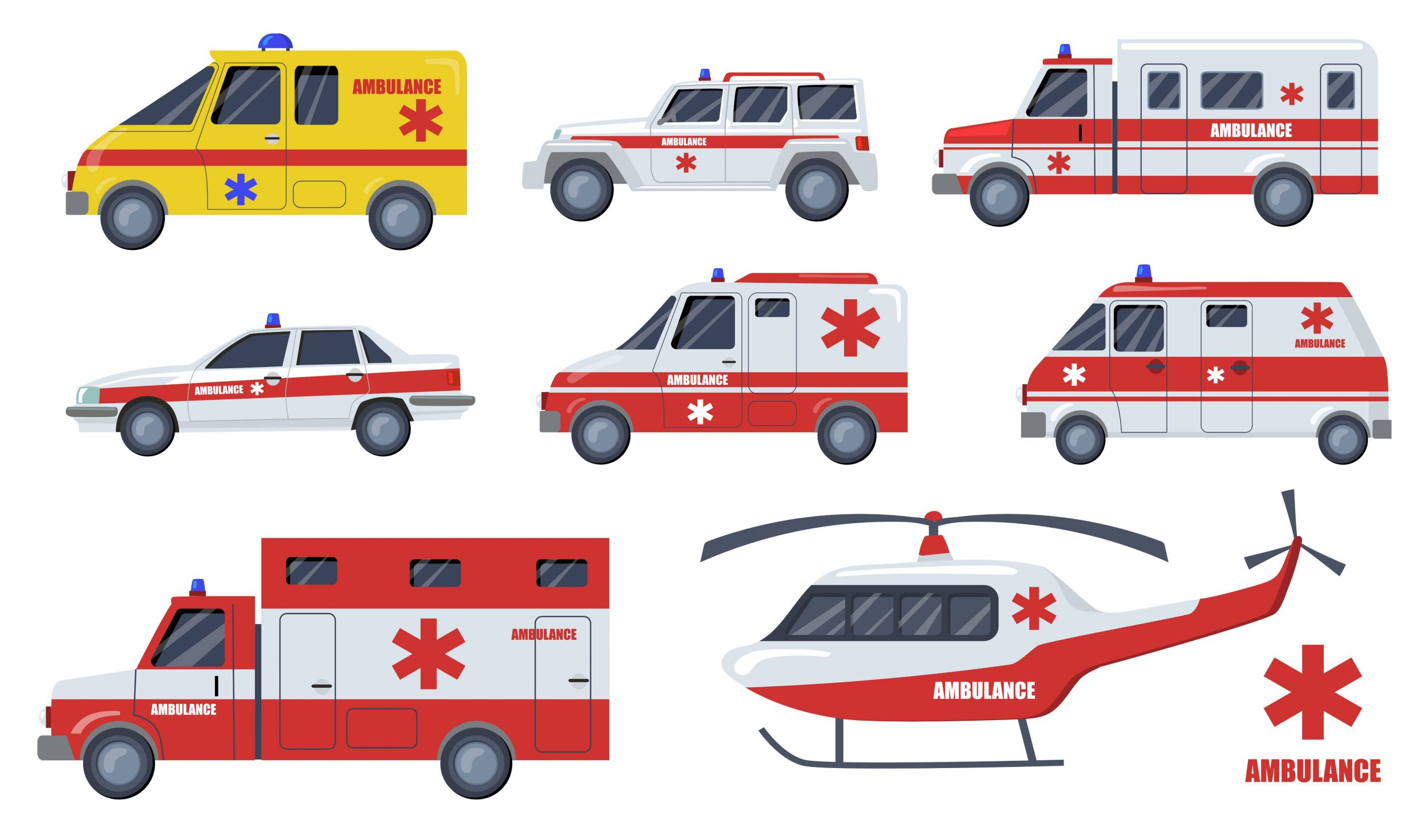
Hop aboard the ambulance express! Journey through India’s diverse fleet of lifesaving vehicles. From rapid responders to mobile medics, explore the significance of each variety in providing timely healthcare. Get ready to unravel the vital role they play in saving lives across the nation.
Types of Ambulances in India
- Basic Life Support (BLS) Ambulances:
- Advanced Life Support (ALS) Ambulances:
- Mobile Intensive Care Unit (MICU) Ambulances:
- Air Ambulance:
The first line of defense in emergencies, BLS ambulances are equipped with essential medical equipment and trained personnel to provide immediate care. They offer basic life-saving interventions like CPR, oxygen administration, and wound management.
ALS ambulances go beyond basic care and provide advanced medical interventions. They feature advanced equipment, such as cardiac monitors, defibrillators to restore normal heartbeat, and ventilators, along with highly skilled paramedics capable of administering medications and conducting advanced procedures.
Designed to mimic a fully functional hospital ICU on wheels, MICU ambulances are equipped with state-of-the-art medical equipment and are staffed by a specialized medical team. They offer critical care interventions, including cardiac monitoring, ventilator support, and advanced medication administration.
Taking healthcare to the skies, air ambulances provide rapid transportation for critical patients over long distances or in remote areas. Equipped with advanced medical equipment, these aircraft are staffed by specialized medical teams who can deliver emergency medical care while in transit, ensuring timely and life-saving interventions.
Importance of Ambulance Services
Ambulance services are a vital component of emergency healthcare systems, serving as the first line of defense in critical situations. Their primary objective is to transport patients to medical facilities swiftly and safely. Equipped with advanced medical equipment and staffed by skilled healthcare professionals, ambulances provide immediate medical attention and support during transit. This immediate response and on-the-spot care can be life-saving, particularly in cases where every minute counts, such as heart attacks, severe injuries, or other medical emergencies.
Beyond transportation, ambulances also play a critical role in stabilizing patients and initiating necessary medical interventions. Paramedics and emergency medical technicians (EMTs) are trained to assess and provide initial treatment to patients at the scene, including administering CPR, managing bleeding, or providing oxygen support. Their presence ensures that patients receive crucial medical care during transit, optimizing their chances of survival and minimizing the risk of further complications.
Challenges Faced by Ambulance Services in India
Ambulance services in India face several challenges that hinder their efficiency and effectiveness. These challenges include:
- Traffic congestion:
- Lack of awareness and infrastructure:
- Insufficient resources:
- Funding and financial constraints:
- Coordination and communication:
- Safety concerns:
Heavy traffic and congested roads often delay ambulance response times, making it challenging to reach patients quickly, especially in urban areas.
Many people are unaware of how to access ambulance services during emergencies. Additionally, inadequate infrastructure, such as poorly maintained roads or inaccessible areas, can pose significant challenges for ambulance operations.
Ambulance services often struggle with limited resources, including medical equipment, and trained staff. This shortage can impact their ability to provide timely and appropriate care.
Ambulance services require sustained funding to maintain their operations, but limited financial resources can hinder their ability to upgrade equipment, maintain vehicles, and provide quality training to their staff.
Effective coordination between ambulance services, hospitals, and emergency response systems is crucial. Challenges in communication and coordination can lead to delays or mismanagement during emergencies.
Ambulance personnel face safety risks while navigating through traffic, dealing with aggressive drivers, or encountering unsafe areas. Ensuring the safety of both patients and ambulance staff is a significant challenge.
Conclusion
Ambulance services are the lifeline of emergency healthcare, providing critical support when time is of the essence. The world of emergency medical services has witnessed tremendous advancements, with Medulance leading the charge. By harnessing technology and innovation, Medulance has revolutionized the way we perceive and access ambulance services. With their commitment to efficiency, promptness, and patient-centric care, Medulance has set a new standard in the industry.